Ever had that unsettling feeling after a fall, a sporting mishap, or even an unexpected bump, where your jaw just doesn’t feel right? It’s a common worry, and for good reason. Your jaw, an incredibly complex and crucial part of your face, is responsible for so many everyday actions – talking, eating, even just expressing emotions. So, when something feels off, it’s only natural to be concerned. Today, we’re going to dive deep into a topic that can sometimes be overlooked but is incredibly important: broken jaw symptoms.
Understanding the signs of a broken jaw isn’t about panicking; it’s about empowering yourself with knowledge. It’s about knowing what to look for, what to do, and most importantly, when to seek professional help. Because when it comes to an injury like this, timely and appropriate medical attention can make all the difference in your recovery journey.
Why Your Jaw Matters So Much

Before we get into the nitty-gritty of broken jaw symptoms, let’s take a moment to appreciate your jaw. Scientifically known as the mandible, it’s the largest and strongest bone in your face. It forms the lower part of your skull, articulates with the temporal bone (just in front of your ear) at the temporomandibular joints (TMJs), and houses your lower teeth. This remarkable structure allows for a wide range of movements, making it essential for chewing, speaking, and even breathing. Given its exposed position and constant use, it’s unfortunately susceptible to injury.
What Causes a Broken Jaw?
A broken jaw, or a mandibular fracture, usually results from significant trauma. Think about the kinds of forces that could disrupt such a strong bone:
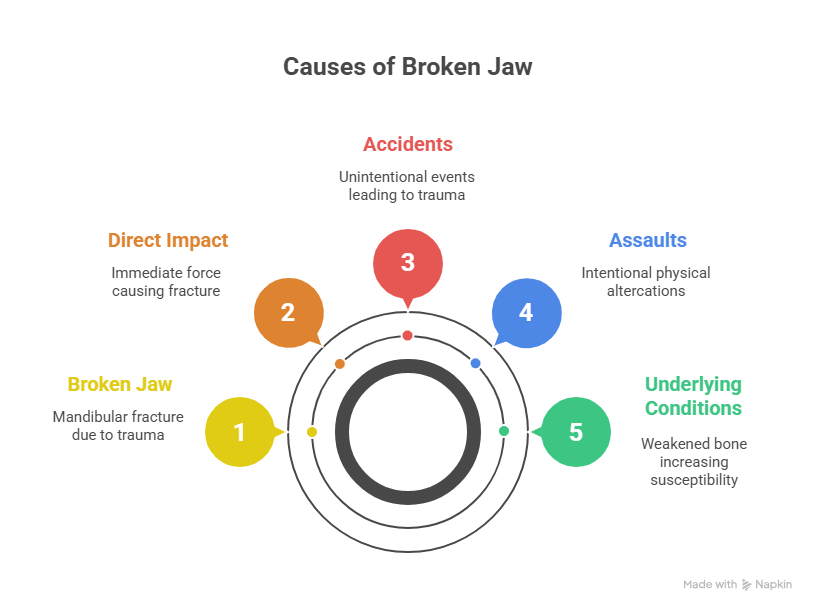
- Direct Impact: This is the most common culprit. A direct blow to the jaw, whether from a punch, a fall, a car accident, or an impact during sports (like football, hockey, or cycling), can easily lead to a fracture.
- Sports Injuries: High-contact sports carry an inherent risk of facial trauma. Even with protective gear, a sudden impact can be enough.
- Motor Vehicle Accidents: The force involved in car crashes often leads to various facial fractures, including the jaw.
- Falls: Tripping and falling, especially onto a hard surface, can result in your chin or jaw taking the brunt of the impact.
- Assaults: Sadly, physical altercations are a significant cause of jaw fractures.
- Workplace Accidents: Certain occupations, particularly those involving heavy machinery or construction, can present risks of facial injury.
Sometimes, underlying conditions can weaken the jawbone, making it more susceptible to fracture from less severe trauma. However, for most people, a broken jaw is the result of a considerable, acute force.
Unpacking Broken Jaw Symptoms: What to Look For
Now, let’s get down to the core of it: broken jaw symptoms. If you’ve experienced any kind of trauma to your jaw area, it’s crucial to be aware of these signs. They can range from subtle discomfort to excruciating pain, and recognizing them quickly is key.
1. Immediate and Severe Pain: This is almost always the first and most prominent symptom. If your jaw is broken, you’ll likely experience intense pain at the site of the fracture. This pain will often worsen when you try to move your jaw, speak, or chew. It might radiate to your ear, neck, or even the side of your head. Don’t dismiss persistent or severe jaw pain after an injury – it’s a critical warning sign.
2. Swelling and Bruising: After a jaw injury, swelling usually develops rapidly around the affected area. This is your body’s natural response to trauma and inflammation. Along with swelling, you’ll likely see bruising (discoloration of the skin) due to ruptured blood vessels beneath the surface. The extent of swelling and bruising can give you an idea of the severity of the injury.
3. Difficulty Opening or Closing Your Mouth: This is a hallmark broken jaw symptom. If your jawbone is fractured, its normal movement will be impaired. You might find it incredibly difficult or even impossible to fully open or close your mouth. Any attempt to do so could cause sharp, shooting pain. Your jaw might feel “stuck” or misaligned.
4. Misalignment of Your Jaw or Teeth: Look in the mirror. Does your jaw look different? Does it seem to be shifted to one side? Are your teeth no longer lining up properly when you try to close your mouth (a condition called malocclusion)? This visual cue is a strong indicator of a fractured jaw. If your bite feels “off” or you can’t bring your teeth together as you normally would, seek immediate medical attention.
5. Numbness or Tingling: A fractured jaw can sometimes damage nearby nerves, leading to numbness or a tingling sensation in your chin, lower lip, or even your teeth. This is because the inferior alveolar nerve, which provides sensation to these areas, runs through the jawbone. If you notice any altered sensation, it’s a significant broken jaw symptom that needs investigation.
6. Bleeding: If the injury caused a laceration (cut) on your skin or inside your mouth, you might experience bleeding. Bleeding from the gums or around the teeth can also indicate a jaw fracture, especially if teeth have been displaced or damaged.
7. Pain When Chewing or Talking: Even if you can somewhat move your jaw, the act of chewing or speaking will likely exacerbate the pain dramatically. This is because these actions put stress on the injured bone. You might find yourself avoiding food and struggling to articulate words.
8. Jaw Stiffness or Locking: Your jaw might feel incredibly stiff, making any movement uncomfortable. In some cases, it might even feel like it’s “locked” in a certain position, making it impossible to open or close it fully.
9. Loose or Missing Teeth: The force that breaks your jaw can also damage your teeth. You might find that some of your teeth are loose, chipped, or even completely knocked out. If teeth are missing, make sure to try and locate them, as sometimes they can be re-implanted if done quickly.
10. Difficulty Swallowing: The pain and swelling associated with a broken jaw can make swallowing incredibly difficult and uncomfortable.
11. Lumps or Deformity: Gently feel your jawbone (if pain allows and you’re careful). Do you feel any unusual bumps, indentations, or a noticeable deformity compared to the other side of your face? This could indicate a fracture. However, do not press hard or try to manipulate the jaw yourself.
12. Ear Pain or Ringing in the Ears: While less common, some individuals with a broken jaw might experience pain in or around the ear, or even ringing in the ears (tinnitus), due to the close proximity of the jaw joint to the ear.
When to See a Doctor: Don’t Delay!
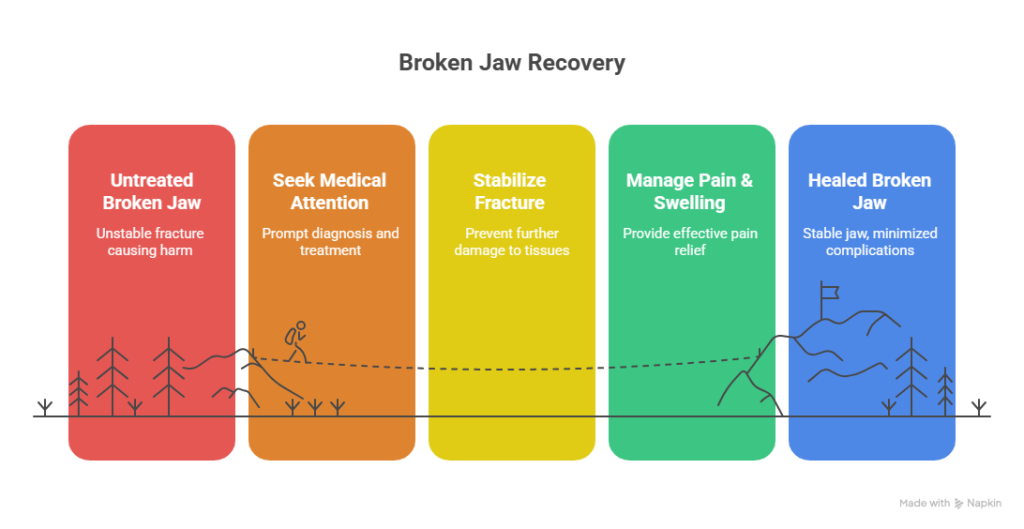
Okay, so you’ve reviewed the broken jaw symptoms. If you suspect you or someone you know has a broken jaw, the absolute most important takeaway is this: seek immediate medical attention. This isn’t an injury you can “wait and see” with. Prompt diagnosis and treatment are crucial for several reasons:
- Preventing Further Damage: An unstable fracture can cause more harm to surrounding tissues, nerves, and blood vessels if not stabilized.
- Optimizing Healing: Early intervention leads to better alignment and a more successful healing process, minimizing complications.
- Managing Pain and Swelling: Medical professionals can provide effective pain relief and manage swelling.
- Addressing Complications: A broken jaw can sometimes lead to airway obstruction (due to swelling or backward displacement of the tongue), infection, or permanent nerve damage if not treated.
Where to Go?
- Emergency Room (ER): For any suspected broken jaw, especially if symptoms are severe, there’s significant bleeding, or you suspect difficulty breathing, head to the nearest emergency room immediately.
- Oral and Maxillofacial Surgeon: Once the initial emergency is handled, you will likely be referred to an oral and maxillofacial surgeon (OMS). These specialists are uniquely trained in diagnosing and treating injuries, diseases, and defects of the mouth, jaw, and face. They are the experts when it comes to managing fractured jaws.
What to Expect at the Doctor’s Office
When you arrive at the medical facility, here’s a general idea of what will happen:
- Medical History and Physical Examination: The doctor will ask about how the injury occurred and your symptoms. They will then carefully examine your face, jaw, and mouth, looking for swelling, bruising, deformities, and checking your bite.
- Imaging Tests: This is where the diagnosis is confirmed. You’ll likely undergo imaging tests such as:
- X-rays: Standard X-rays can often reveal the location and type of fracture.
- CT Scan (Computed Tomography): A CT scan provides more detailed, three-dimensional images of the bones and surrounding tissues, which is particularly useful for complex fractures or when planning surgery.
Treatment Options for a Broken Jaw
Treatment for a broken jaw depends entirely on the severity and location of the fracture. The goal is always to restore proper alignment of the jaw and allow it to heal correctly.
- Non-Surgical Treatment (Conservative Management):
- Jaw Immobilization (Wiring the Jaw): For many stable fractures, the jaw needs to be immobilized to allow the bones to heal without movement. This often involves “wiring” the upper and lower teeth together, keeping the jaw shut for several weeks (typically 4-8 weeks). This sounds daunting, but it’s often the most effective way for the bones to fuse properly.
- Liquid Diet: While your jaw is wired shut, you’ll be on a strictly liquid or soft diet. Think smoothies, pureed soups, nutritional shakes, and other easy-to-consume foods.
- Pain Management: Your doctor will prescribe pain medication to help manage discomfort.
- Antibiotics: To prevent infection, especially if there are open wounds or a fracture extends into the mouth, antibiotics may be prescribed.
- Jaw Immobilization (Wiring the Jaw): For many stable fractures, the jaw needs to be immobilized to allow the bones to heal without movement. This often involves “wiring” the upper and lower teeth together, keeping the jaw shut for several weeks (typically 4-8 weeks). This sounds daunting, but it’s often the most effective way for the bones to fuse properly.
- Surgical Treatment:
- Open Reduction and Internal Fixation (ORIF): For more complex or unstable fractures, surgery may be necessary. During ORIF, the surgeon will make an incision (either inside the mouth or on the skin) to access the fracture site. They will then realign the bone fragments and secure them in place using small metal plates and screws. These plates and screws are usually made of titanium and are designed to remain in your body permanently, unless they cause issues later on.
- Bone Grafting: In very severe cases where there’s significant bone loss, a bone graft (using bone from another part of your body or a synthetic material) might be necessary to help bridge the gap and promote healing.
- Open Reduction and Internal Fixation (ORIF): For more complex or unstable fractures, surgery may be necessary. During ORIF, the surgeon will make an incision (either inside the mouth or on the skin) to access the fracture site. They will then realign the bone fragments and secure them in place using small metal plates and screws. These plates and screws are usually made of titanium and are designed to remain in your body permanently, unless they cause issues later on.
Life During Recovery
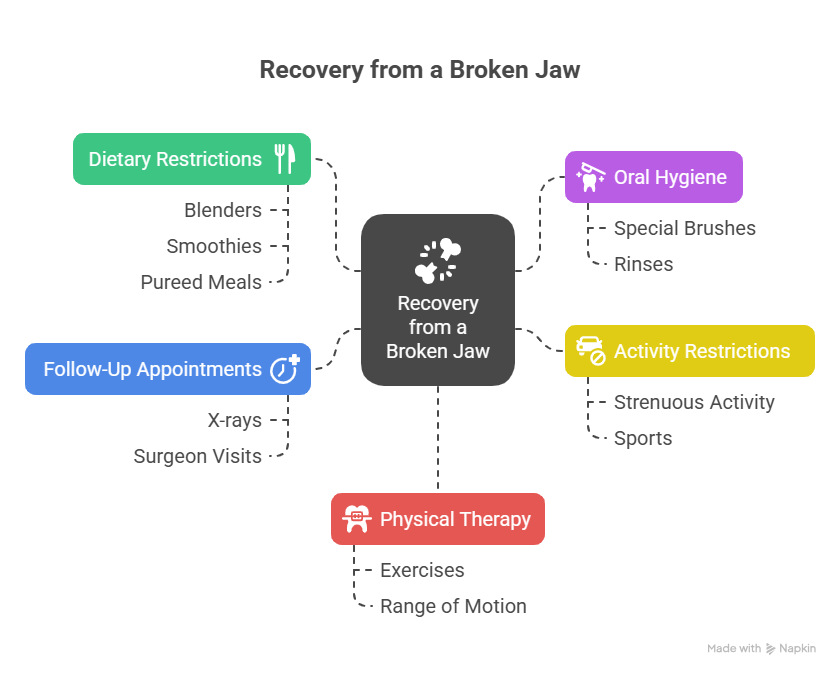
Recovering from a broken jaw requires patience and adherence to your doctor’s instructions.
- Dietary Restrictions: This is perhaps the most challenging aspect for many. Whether your jaw is wired shut or you’ve had surgery, a soft or liquid diet will be your reality for weeks. Get creative with blenders and explore new recipes for nutrient-rich smoothies and pureed meals.
- Oral Hygiene: Maintaining excellent oral hygiene is paramount, especially if your jaw is wired. Your doctor or dental professional will show you how to clean your mouth effectively, often involving special brushes and rinses.
- Activity Restrictions: You’ll need to avoid strenuous activity and any sport that could put your jaw at risk of re-injury.
- Follow-Up Appointments: Regular follow-up appointments with your oral and maxillofacial surgeon are crucial to monitor healing progress. They will take follow-up X-rays to ensure the bones are uniting properly.
- Physical Therapy: Once the jaw has healed sufficiently, you might need physical therapy to regain full range of motion and strength in your jaw muscles. This could involve specific exercises to stretch and strengthen the jaw.
Complications to Watch For
While most broken jaws heal well with proper treatment, it’s good to be aware of potential complications:
- Infection: Any open wound or surgical site carries a risk of infection. Follow all post-operative care instructions carefully.
- Non-Union or Malunion: In some cases, the bones may not heal properly (non-union) or may heal in an incorrect position (malunion), requiring further intervention.
- Nerve Damage: While often temporary, nerve damage can sometimes be permanent, leading to persistent numbness or altered sensation.
- TMJ Problems: The temporomandibular joints can sometimes be affected by a jaw fracture, leading to chronic pain, clicking, or limited movement.
- Scarring: If an external incision was made, there will be a scar, though surgeons strive to make them as discreet as possible.
Preventing Jaw Injuries
While accidents happen, there are certainly steps you can take to reduce your risk of a jaw fracture:
- Wear Protective Gear: If you participate in contact sports, always wear a properly fitted mouthguard and, if appropriate, a helmet with a face shield.
- Seatbelts and Airbags: Always wear your seatbelt in a vehicle. Airbags provide crucial protection in the event of a crash.
- Address Fall Hazards: Be mindful of slippery surfaces, loose rugs, and poor lighting that could lead to falls.
- Avoid Physical Confrontations: Steer clear of situations that could escalate into violence.
Final Thoughts and When to Seek Expert Help
Understanding broken jaw symptoms is the first step in protecting your health. If you experience any of the signs we’ve discussed after an injury, don’t hesitate. Your jaw is too important to leave to chance.
For expert care and comprehensive treatment of jaw injuries, including complex fractures, you’ll want to consult with a specialist. Professionals like Dr. Suresh are highly skilled in diagnosing and treating conditions of the jaw and face, ensuring you receive the best possible care for a swift and effective recovery. For more information and to explore the services offered, you can visit https://gnathosface.com/. Remember, when it comes to your health, getting the right diagnosis from an experienced professional like Dr. Suresh is absolutely vital.
Frequently Asked Questions (FAQs) About Broken Jaw Symptoms
Here are some common questions people have about broken jaws:
How long does it take for a broken jaw to heal?
The healing time for a broken jaw varies depending on the severity and type of fracture, as well as the individual’s overall health. Generally, an uncomplicated fracture can take 4 to 8 weeks to heal sufficiently for the wires to be removed (if applicable) or for the plates and screws to fully integrate. Complete healing and return to normal function can take several months, often requiring physical therapy.
Can I eat solid food with a broken jaw?
No, absolutely not, especially if your jaw is wired shut or you’ve just undergone surgery. You will be on a strictly liquid or very soft, pureed diet for the duration of your healing. This is crucial to prevent any movement that could disrupt the healing process. Your doctor will provide specific dietary guidelines.
Will my jaw be wired shut if it’s broken?
It depends on the type and stability of the fracture. Many, but not all, broken jaws require intermaxillary fixation, commonly known as “wiring the jaw shut,” to immobilize the bone fragments and allow them to heal. For some fractures, especially those treated with plates and screws during surgery, wiring may not be necessary or might only be for a shorter period. Your oral and maxillofacial surgeon will determine the best approach for your specific injury.
Will my jaw be wired shut if it’s broken?
It depends on the type and stability of the fracture. Many, but not all, broken jaws require intermaxillary fixation, commonly known as “wiring the jaw shut,” to immobilize the bone fragments and allow them to heal. For some fractures, especially those treated with plates and screws during surgery, wiring may not be necessary or might only be for a shorter period. Your oral and maxillofacial surgeon will determine the best approach for your specific injury.
What should I do immediately after a suspected jaw injury?
If you suspect a broken jaw, first try to remain calm. Do not attempt to move your jaw or manipulate it. Apply a cold compress to the injured area to help reduce swelling. If there’s bleeding, apply gentle pressure with a clean cloth. Seek immediate medical attention by going to the nearest emergency room. Avoid eating or drinking anything, as you might need emergency surgery.
Are there long-term effects of a broken jaw?
With proper treatment and adherence to recovery protocols, most people recover fully from a broken jaw. However, potential long-term effects can include chronic pain (especially if the fracture involved the TMJ), persistent numbness or altered sensation if nerve damage occurred, difficulty with full jaw movement, or bite irregularities. Regular follow-up with your surgeon and physical therapy can help minimize these risks.
How painful is a broken jaw?
A broken jaw is typically very painful, with the pain worsening significantly with any attempt to move the jaw, speak, or chew. The pain level can vary depending on the severity of the fracture, but it’s generally described as intense and persistent. Pain medication will be prescribed to manage this discomfort during the healing process.