If you’re reading this, you’re likely experiencing some uncomfortable, nagging pain or stiffness around your jaw, and you’re wondering if it might be a TMJ disorder. That acronym, TMJ, stands for the Temporomandibular Joint—the complex hinges that connect your lower jaw to your skull, right in front of your ears. When people talk about a “TMJ problem,” they’re usually referring to Temporomandibular Disorders, or TMD. These aren’t just one single issue but a group of conditions that cause pain and dysfunction in your jaw joint and the muscles that control jaw movement.
It’s a frustrating situation because TMD can interfere with simple daily activities like talking, eating, and even smiling comfortably. The symptoms are often confusing, radiating to the head, neck, and ears, leading many people to seek help from multiple specialists before getting an accurate diagnosis.
Today, we’re going to give you a comprehensive guide to understanding this common yet complex issue. We’ll dive into what are the common signs of TMJ disorders and how are they treated, breaking down the clues your body is giving you and outlining the effective paths to finding relief. Let’s get to the core of this discomfort and explore the journey to restoring your jaw health!
Understanding the TMJ: The Body’s Most Unique Joint
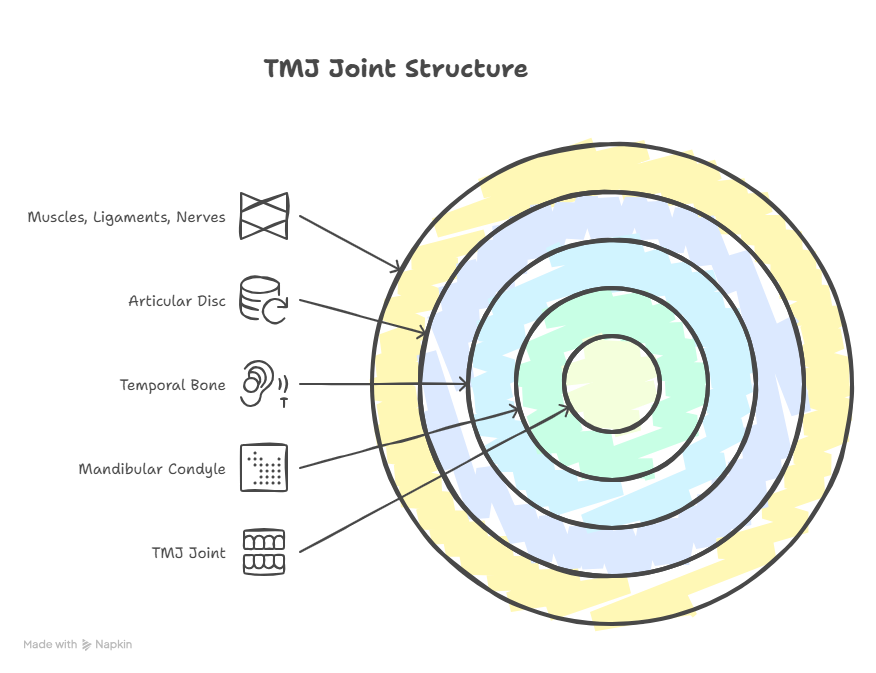
Before we explore the signs of the disorder, let’s appreciate the joint itself. The TMJ is one of the most unique and constantly used joints in the body. Unlike the simple hinge of your knee, your TMJ functions like a complex sliding hinge. This allows for both the simple up-and-down movement of biting and the side-to-side and forward motions needed for chewing and grinding food.
Each joint (you have two, one on each side) consists of:
- The Mandibular Condyle: The rounded end of the lower jawbone.
- The Temporal Bone: The socket where the condyle rests.
- The Articular Disc: A small, shock-absorbing piece of cartilage between the two bones, ensuring smooth movement.
- Muscles, Ligaments, and Nerves: A surrounding network that powers and stabilizes the joint.
A TMJ disorder arises when there is a problem with the joint itself, the surrounding muscles, or the associated nerves.
Struggling with Jaw Pain or Clicking Sounds?
TMJ disorders can cause chronic pain, headaches, and difficulty in jaw movement. Get an accurate diagnosis and a personalized treatment plan from our specialist TMJ surgeons to restore comfort and function faster.
Book Your TMJ ConsultationCommon Signs of TMJ Disorders: What Are the Common Signs of TMJ Disorders?
The symptoms of TMD are incredibly varied, which is why the condition is sometimes called “The Great Imposter.” They can be localized to the jaw or radiate widely across the head and neck. Here are the most common signs you should look out for:
1. Pain and Tenderness
- Jaw Pain: This is the most common symptom. The pain can be a dull, constant ache or a sharp, intense pain that comes and goes. It is often felt in the jaw joint itself (just in front of the ear) or in the surrounding muscles of the face and temples.
- Facial Pain: The pain may spread beyond the jaw, affecting the cheeks and the entire side of the face.
- Headaches: Frequent headaches, often resembling tension headaches, are very common. They are typically felt in the temples, forehead, or the back of the skull, and often worsen with jaw movement or stress.
- Neck and Shoulder Pain: The large muscles that control the jaw are connected to the neck and shoulder muscles. Tension and spasms in the jaw can easily radiate down, causing chronic neck stiffness and shoulder aches.
2. Auditory Symptoms (Ear Trouble)
The proximity of the TMJ to the ear canal and middle ear structures leads to many confusing ear-related symptoms, often leading patients to an Ear, Nose, and Throat (ENT) specialist first.
- Earache: Pain felt inside or around the ear that is not caused by an ear infection. This is a classic example of referred pain from the nearby joint or tense muscles.
- Tinnitus: A persistent ringing, buzzing, or hissing sound in the ears.
- Feeling of Fullness: A sensation of pressure or blocked ears, often without any corresponding cold or congestion.
3. Jaw Function Issues
These mechanical issues are often the clearest indicators of a physical joint problem.
- Clicking, Popping, or Grating Sounds: This is the second most common sign. These sounds occur when the articular disc is displaced and snaps in and out of place as you open or close your mouth. A harsh, grinding sound, called crepitus, often indicates bone-on-bone friction due to joint wear (osteoarthritis).
- Limited Jaw Movement: You may find it difficult or painful to open your mouth fully or wide enough to comfortably take a large bite or yawn.
- Jaw Locking: The jaw may momentarily get stuck in an open or closed position, which can be frightening and painful. This often occurs when the disc gets fully stuck out of position.
- Deviation or Deflection: When you open your mouth, your jaw may track unevenly, moving in an S-curve (deviation) or consistently shifting to one side (deflection).
4. Bite Changes
- Malocclusion Feeling: You may suddenly feel that your teeth don’t fit together correctly or that your bite feels “off.” This can happen if the position of the mandibular condyle in the joint socket shifts due to muscle tension or disc displacement.
- Tooth Sensitivity/Wear: Excessive clenching or grinding (bruxism), which is often a cause or symptom of TMD, can lead to severe tooth wear, sensitivity, and even fractures.
Diagnosis: Pinpointing the Problem
Getting a precise diagnosis is the most important step in treating a TMJ disorder. Since the causes are diverse (muscle, joint, or bone), a one-size-fits-all treatment rarely works.
An Oral and Maxillofacial Surgeon (OMS) or an Orofacial Pain Specialist is often the best choice for diagnosis. They will:
- Take a Comprehensive History: Reviewing your trauma history, stress levels, habits (like clenching), and dental history.
- Conduct a Physical Examination: Palpating your jaw muscles and joints, listening for sounds, and measuring your jaw’s range of motion.
- Use Advanced Imaging:
- Panoramic X-rays: To check the overall structure of the jawbones and teeth.
- CT Scans (Computed Tomography): To visualize the bony structure of the joint for signs of arthritis or damage.
- MRI (Magnetic Resonance Imaging): The gold standard for visualizing the soft tissues, particularly the position and condition of the articular disc.
This thorough evaluation helps the doctor classify your TMD as primarily a muscle issue (myofascial pain), a joint issue (internal derangement), or a degenerative joint issue (osteoarthritis).
Treatment Options: How Are TMJ Disorders Treated?
The good news is that most cases of TMD (around 80-90%) respond well to conservative, non-surgical treatments. Surgery is typically reserved for severe structural joint damage that has failed to improve with extensive non-surgical therapy.
1. Conservative (Non-Surgical) Treatments
This is always the first line of defense. The goal is to reduce pain, relax muscles, and restore normal jaw function.
- Self-Care and Lifestyle Modification:
- Soft Diet: Avoid hard, crunchy, and chewy foods (like gum, hard nuts, caramels) to rest the jaw muscles.
- Moist Heat/Ice: Apply moist heat to tight, sore muscles (cheeks and temples) or ice packs to the joint area to reduce inflammation.
- Stress Management: Since stress often leads to clenching, practicing relaxation techniques like meditation, deep breathing, and light stretching is vital.
- Limit Excessive Jaw Movement: Avoid wide yawning and resting your chin on your hand.
- Medications:
- NSAIDs: Over-the-counter Non-Steroidal Anti-Inflammatory Drugs (like ibuprofen) to reduce pain and inflammation.
- Muscle Relaxants: Prescription medications to alleviate severe muscle spasms and tension, often taken at night.
- Low-Dose Antidepressants: These are sometimes prescribed not for depression, but because they can help control pain signals and improve sleep quality at night, which reduces clenching.
- Oral Appliances (Splints/Night Guards):
- These custom-made acrylic devices are worn over the upper or lower teeth, often at night. They work by preventing teeth clenching and grinding, protecting the teeth, and in some cases, helping to stabilize the jaw joint disc. They are essential for managing bruxism-related TMD.
- Physical Therapy:
- A specialized physical therapist can teach you gentle stretches, postural correction exercises, and techniques to restore normal joint mechanics and relieve muscle tightness.
Struggling with Jaw Pain or Clicking Sounds?
TMJ disorders can cause chronic pain, headaches, and difficulty in jaw movement. Get an accurate diagnosis and a personalized treatment plan from our specialist TMJ surgeons to restore comfort and function faster.
Book Your TMJ Consultation2. Interventional and Minimally Invasive Treatments
If conservative treatments fail, the next step involves in-office procedures performed by a specialist.
- Injections:
- Trigger Point Injections: Injecting a local anesthetic into tight, painful muscle knots (trigger points) to relieve spasms.
- Corticosteroid Injections: Injecting a steroid into the joint space to reduce inflammation and pain caused by arthritis or synovitis.
- Botulinum Toxin Injections: Injecting BOTOX into the powerful chewing muscles (like the masseter) to temporarily weaken them, significantly reducing clenching and muscle strain. This can offer profound relief for chronic muscle pain.
- Arthrocentesis:
- A minimally invasive procedure where a specialist flushes the joint space with sterile fluid. This helps remove inflammatory byproducts, lubricate the joint, and sometimes helps unstick a displaced disc, improving mobility and reducing pain.
3. Surgical Treatments
Surgery is only considered for a small percentage of patients (less than 10%) who have confirmed structural joint damage (e.g., severe arthritis, perforated disc, bony fusion) that has not responded to any other treatment.
- Arthroscopy: A minimally invasive surgery using a tiny camera (arthroscope) inserted into the joint. The surgeon can visualize the joint, remove adhesions, smooth rough surfaces, and, in some cases, repair or reposition the disc. Recovery is significantly shorter than open surgery.
- Open-Joint Surgery (Arthroplasty): A traditional surgery used for extensive repair, such as removing damaged bone, repositioning a severely displaced disc, or performing a joint reconstruction.
- Total Joint Replacement: Reserved for extremely rare cases where the joint is severely and irreversibly damaged, often due to aggressive arthritis or trauma. The TMJ is replaced with a custom prosthetic joint.
Finding the Right Specialist
When dealing with something as complex as jaw and facial pain, having an expert guide is essential. Because TMD involves muscles, joints, and teeth, the best results often come from a specialist with comprehensive training.
An Oral and Maxillofacial Surgeon (OMS), like Dr. Suresh, possesses the dual training in dentistry and medicine, along with extensive surgical residency experience, to accurately diagnose the source of the pain—whether it’s muscular tension, internal joint derangement, or a bite problem. They are uniquely qualified to offer the full spectrum of care, from custom splints and injections to complex TMJ surgery.
For a precise diagnosis and a truly personalized treatment plan tailored to your specific form of TMD, it is crucial to consult with a specialist who understands the intricate biomechanics of your head and neck. Professionals like Dr. Suresh are dedicated to using advanced diagnostic techniques and offering effective solutions to help you achieve lasting relief and restore your quality of life. To learn more about how Dr. Suresh and his team can help you overcome your TMJ disorder. Don’t let jaw pain control your life—take the next step toward comfort and function.
Struggling with Jaw Pain or Clicking Sounds?
TMJ disorders can cause chronic pain, headaches, and difficulty in jaw movement. Get an accurate diagnosis and a personalized treatment plan from our specialist TMJ surgeons to restore comfort and function faster.
Book Your TMJ ConsultationFrequently Asked Questions (FAQs) About TMJ Disorders
Does jaw clicking always mean I have a serious TMJ disorder?
No, jaw clicking does not always mean you have a serious TMJ disorder, as occasional, painless clicking is relatively common and often requires no treatment. However, if the clicking is accompanied by pain, a limited ability to open your mouth, or an occasional feeling of the jaw locking, it is a sign of internal joint derangement that warrants professional evaluation.
Is a night guard the only way to treat a TMJ disorder?
A custom-made oral appliance (night guard or splint) is one of the most common and effective ways to manage a TMJ disorder, especially those related to teeth clenching and grinding, but it is not the only treatment. Effective management often involves a combination of therapies, including pain medication, specialized physical therapy, stress reduction, and dietary modifications.
Can I completely cure a TMJ disorder, or is it just managed?
Many TMJ disorders, particularly those related to muscle tension and stress, can be completely cured or resolved by implementing effective self-care, using an oral appliance, and managing stress. However, if the disorder involves joint arthritis or disc degeneration, the condition is often managed long-term to keep pain under control and preserve function.
Why do TMJ problems cause neck and shoulder pain?
TMJ problems cause neck and shoulder pain because the muscles responsible for chewing and keeping the jaw stable are closely connected to the muscles in the temples, head, and neck. When the jaw muscles are constantly strained or in spasm due to clenching or joint dysfunction, the tension radiates downward, creating trigger points and pain in the neck and shoulders.
How long does it usually take for TMJ treatment to start providing relief?
The timeline for relief varies, but most patients with muscular TMJ pain will notice a reduction in symptoms within a few weeks of consistently using a custom oral appliance, taking prescribed muscle relaxants, and applying self-care techniques like heat therapy. For joint-related pain, interventions like joint injections or arthrocentesis can often provide significant relief more quickly.
When should I consider seeing an Oral and Maxillofacial Surgeon for my TMJ symptoms?
You should consider seeing an Oral and Maxillofacial Surgeon when conservative treatments prescribed by your dentist haven’t provided lasting relief, or if your symptoms include frequent jaw locking, severe, persistent joint pain, or significant structural issues visible on an MRI, as an OMS is the specialist most qualified to diagnose complex joint issues and perform advanced, minimally invasive or open-joint surgical treatments.